Características epidemiológicas y quirúrgicas en pacientes con secuelas de enfermedad de Fournier
Palabras clave:
gangrena de Fournier, colgajos, cirugía reconstructivaResumen
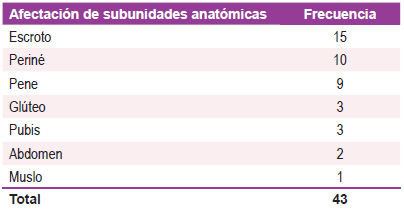
Introducción: La gangrena de Fournier actualmente se define como una forma específica de fascitis necrotizante sinérgica, rápida, progresiva y de origen multibacteriano, que afecta principalmente la fascia muscular de región perineal, genital o perianal e incluso de pared abdominal; con punto de partida genitourinario, colorrectal o idiopático. Todo ello, acompañado de gangrena de piel de estas áreas debida a trombosis de vasos sanguíneos subcutáneos. Objetivos: Describir las características epidemiológicas y quirúrgicas de los pacientes secuelares de la enfermedad de Fournier en la Unidad de Cirugía Plástica del Hospital de Clínicas en un período de 2 años. Materiales y métodos: Estudio observacional, descriptivo, de corte transversal, temporalmente retrospectivo, tipo serie de casos. El tipo de muestreo fue no probabilístico a conveniencia. Se presentan 18 pacientes secuelares de enfermedad de Fournier reconstruidos en la Unidad de Cirugía Plástica de Hospital de Clínicas entre los años 2020 y 2021. Resultados: Durante el periodo del estudio se realizaron 395 cirugías en el Servicio de Cirugía Plástica del Hospital de Clínicas, de los cuales 18 pacientes fueron intervenidos quirúrgicamente por secuelas de enfermedad de Fournier, lo que representa el 5% del total. En lo que respecta a las variables demográficas, la edad osciló entre los 37 y 85 años con mayor afectación en la sexta década de la vida con un promedio de 61 años. El 94% de los pacientes fue de sexo masculino; el 89% de los pacientes tenía como patología de base
la diabetes mellitus tipo 2, seguido de la obesidad en el 72% y la hipertensión arterial en el 56% de los casos; el 83% de los casos estuvo afectada la región escrotal seguido de la región perineal con el 56% de los pacientes y el pene en el 50% de los casos. La técnica reconstructiva empleada en mayor frecuencia fueron los colgajos en 10 pacientes, seguido del injerto de piel en 8 pacientes, y el cierre primario en 6 pacientes, cabe mencionar que en algunos pacientes se emplearon varias técnicas reconstructivas siguiendo el concepto de reconstrucción por sub-unidades anatómicas, entre los colgajos los más utilizados fueron el colgajo de perforante de la circunfleja femoral medial (perforante de gracilis) con el 50% de los casos seguido del colgajo de transposición fasciocutáneo de la pudenda interna con el 30%, y por último el colgajo de avance fasciocutáneo con el 20% (Tabla 3). La estancia hospitalaria promedio fue de 3 días, con un mínimo de 1 día y un máximo de 5 días post operatorio. Se reportó como complicación la dehiscencia de sutura en 3 pacientes, no se observó complicaciones en el 77% de los casos. Conclusión: Las secuelas de la enfermedad de Fournier sometidos a cirugías representan el 5% del total de cirugías realizadas en nuestro Servicio, son más prevalentes en la sexta década de la vida, afecta más al sexo masculino con diabetes mellitus tipo 2 como patología de base, las técnicas reconstructivas empleadas en las secuelas son variables de acuerdo a las regiones anatómicas afectadas y pueden abarcar desde el cierre primario hasta la utilización de colgajos para su reparación.
Referencias
Litchfield WR. The bittersweet demise of Herod the Great. J R Soc Med 1998; 91: 283-4.
Nathan B. Fournier’s gangrene: a historical vignette. J Can Surg 1998; 41: 7.
Baurienne H. Sur une plaie contuse qui s’est terminee par le sphacele de le scrotum. J Med Chir Pharm 1764; 20: 251-6. Citado por Smith GL y cols. 5.
Fournier JA. Gangrene foudroyante de la verge. Medecin Pratique 1883; 4: 589-97. Citado por Vick R y cols. 30.
Smith GL, Bunker CB, Dinneen MD. Fournier’s gangrene. Br J Urol 1998; 81: 347-55.
Lamb RC, Juler GL. Fournier’s gangrene of the scrotum. A poorly defined syndrome or a misnomer? Arch Surg 1983; 118: 38-40.
Urdaneta-Carruyo E , Méndez-Parra A, Urdaneta-Contreras A V . Gan- grena de Fournier en la edad pediátrica. Memorias LI Congreso Nacional de Puericultura y Pediatría. Puerto La Cruz, Venezuela, 2005.
Wright AJ, Lall A, Gransden WR, Joyse MR, Rowsell A, Clark G. A case of Fournier gangrene complicating idiopathic nephrotic syndrome of childhood. Pediatr Nephrol 1999; 13: 838-39.
Urdaneta-Carruyo E, Méndez-Parra A, Urdaneta-Contreras A V . Prees- colar con síndrome nefrótico y Gangrena de Fournier en escroto. Memorias VI Congreso Latinoamericano de Nefrología Pediátrica. Valencia, Venezuela, 1999.
Stephens BJ, Lathrop JC, Rice WT, Gruenberg JC. Fournier’s gangrene: historic (1764-1978) versus contemporary (1979-1988) differences in etiology and clinical importance. Am Surg 1993; 59: 149-54.
Baskin LS, Carroll PR, Cattolica EV, Mc Aninch JW. Necrotizing soft tissue infections of the perineum and genitalia. Bacteriology, treatment, and risk assessment. Br J Urol 1990; 65: 524-9.
Walther PJ, Andriani RT, Maggio MI, Carson CC III. Fournier’s gangrene: a complication of penile prosthetic implantation in a renal transplant patient. J Urol 1987; 137: 299-300.
Heurkens AH, Peters WG, van den Broek PJ, Willemze R. Fournier’s gangrene or fulminant necrotizing fasciitis of the scrotum and penis as a complication of granulocytopenia in a patient with acute myelogenous leukemia (AML). Neth J Med 1988; 32 (5-6): 235-9.
Merino E, Boix V, Portilla J, Reus S, Priego M. Fournier’s gangrene in HIV-infected patients. Eur J Clin Microbiol Infect Dis 2001; 20: 910-3.